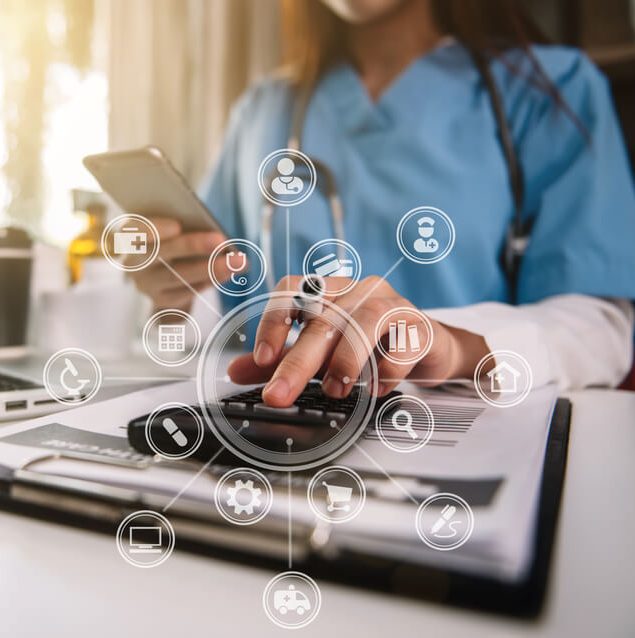
A core component of our Revenue Cycle Management solution is to integrate end-to-end revenue cycle activities with the goal of streamlining reimbursements, increasing cash collections, and reducing the overhead cost associated with medical billing and coding compliance.
Patient Help Desk
Get patient inquiries handled quickly, kindly, and correctly with Billingly CO expert help desk support.
Read MoreMedical Billing
Keep your billing process accurate, secure, and fast with Billingly CO tailored medical billing services
Read MoreMedical Coding
Our medical coding services cover all claims' coding to remove inaccuracies and boost reimbursements
Read MoreMedical Credentialing
Stay compliant and get enrolled faster with Billingly CO streamlined credentialing services.
Read MorePrior Authorization
Speed up approvals and reduce delays with Billingly CO efficient prior authorization support.
Read MoreClaim Submissions
we streamline the claim submission process to ensure fast reimbursements and minimal errors.
Read MoreAt Billingly CO, we redefine excellence in revenue cycle management by combining cutting-edge technology with deep industry expertise. Our mission is to deliver unmatched accuracy, compliance, and revenue optimization for healthcare providers, ensuring every claim is maximized and every dollar is accounted for.
Claim Rate achieved
90%
Clean Claim Rate Achieved
90% Clean Claim Rate: First-pass success for faster reimbursements and fewer denials—maximizing your revenue with precision billing

Accurate billing is the bridge between healthcare and financial clarity

25+ Years Of Experience
Verification
The patient's details, including insurance information and eligibility, are verified with the payer to ensure all necessary data is accurate and up to dat
Read moreSubmission
The completed medical claim is submitted electronically or manually to the insurance payer for review and processing.
Read moreProven billing strategies that reduce denials, accelerate payments, and scale your revenue cycle.
Clean Claim Rate 98%
Collection Ratio 90%
Faster A/R Turnaround 65%
Our power of choice is untrammelled and when nothing prevents being able to do what we like best every pleasure.
Fast Claim Processing
Speed and accuracy are non-negotiable. Our certified team ensures error-free claims are submitted within 48 hours—reducing denials and accelerating your cash flow. Leveraging AI-powered scrubbing and payer-specific rules, we guarantee faster reimbursements so you can focus on patient care
- AI-Driven Error Detection: Catch coding mistakes before submission.
- Payer-Specific Rules: Custom workflows for Medicare, Medicaid, and private insurers.
- Real-Time Tracking: Monitor claim status via our client portal.

MAXIMIZING REVENUE
Unlock hidden revenue with proactive denial prevention, underpayment recovery, and data-driven insights. Our end-to-end revenue cycle management identifies leaks and optimizes every dollar—so you get paid faster and more accurately.
- Denial Prevention: 85%+ appeal success rate with root-cause analysis.
- Underpayment Audits: Recover an average of 12-15% in missed reimbursements.
- Performance Analytics: Custom reports track KPIs like A/R days and net collections.

Optimized RCM
Our end-to-end RCM solutions streamline every touchpoint—from patient registration to final payment—eliminating bottlenecks and maximizing efficiency. With cutting-edge technology and deep industry expertise, we transform your revenue cycle into a well-oiled machine
- End-to-End Integration: Automated workflows from scheduling to collections
- Real-Time Analytics: Dashboard tracks A/R days, denial rates, and cash flow
- Payer Performance Insights: Identify slow-paying insurers and optimize contracts
We partner with healthcare providers, insurers, and technology innovators to deliver seamless revenue cycle solutions. Together, we’re transforming medical billing